Cashless Hospitalization for Cancer Treatment

Why Choose Apollo Hospitals for Cashless Cancer Treatment?
Expertise in Oncology
Apollo Hospitals hosts a team of top oncologists and surgeons, offering specialized and personalized care for all types of cancer.
Advanced Technology
With advanced tools like robotic surgery, precision radiotherapy, and modern chemotherapy, Apollo delivers precise and effective treatments.
Comprehensive Care
From initial diagnosis to rehabilitation, Apollo provides a full range of cancer care services, addressing both medical and emotional needs.
Cashless Hospitalization
Through partnerships with 40 insurance providers and TPAs, Apollo ensures a smooth cashless process, enabling patients to focus on recovery.
Patient-Centric Approach
Apollo emphasizes personalized care, clear communication, and stress-free treatment to provide a comforting experience for every patient.
Leadership in Oncology
As a leader in cancer care, Apollo advances patient outcomes through innovation, research, and cutting-edge therapies.
Insurance Partners & TPAs Of Apollo Hospitals' (As of 11-12-2024)
- Bajaj Allianz General Insurance Co. Ltd
- Care Health Insurance Limited
- Family Health Plan Ltd
- Genins India TPA Ltd
- HDFC ERGO General Insurance Co Ltd
- HEALTHINDIA INSURANCE TPA SERVICES PVT LTD
- ICICI Lombard Health Care
- IFFCO - TOKIO General Insurance Co.Ltd
- MDIndia Healthcare Services (TPA) Pvt. Ltd
- Medi Assist Insurance
- MedSave Healthcare (Tpa) Ltd
- Star Health and Allied Insurance Co. Ltd
- Paramount Health Services TPA Pvt. Ltd
- Raksha TPA Pvt.Ltd
- Reliance General Insurance
- Vidal Health TPA Pvt Ltd
- HI TPA
- CHOLA M S
- TATA AIG
- VIPUL MEDCORP TPA
- GO DIGIT INSURANCE
- Star Health and Allied Insurance Co. Ltd
- NIVA BUPA
- VOLO HEALTH TPA
- HEALTH INDIA TPA
- EASTWEST VANI
- HERITAGE HEALTH TPA
- PARK TPA
- Ericson TPA
- SAFEWAY TPA
- NAVI GENERAL INSURANCE
- LIBERTY GENERAL INSURANCE
- ICICI PRUDENTIAL
- ADITYA BIRLA
- PARK TPA
- ACKO GENERAL INSURANCE
- ROYAL SUNDERAM
- FUTUR GENERALI
- GOOD HEALTH TPA
- SBI GENERAL INSURANCE
Mediclaim Processes You Should Know
- Cashless Process
The insurer directly settles the hospital bills at network hospitals. Pre-authorization is mandatory before planned treatments or within 24 hours for emergencies.
- Reimbursement Process
Patients initially pay the hospital bills and later claim reimbursement by submitting bills, discharge summaries, and prescriptions for verification.
- Hybrid Process
This process combines cashless and reimbursement methods, where some expenses are directly settled, and others are reimbursed later.
- Planned Hospitalization
Pre-authorization ensures smooth cashless claims for scheduled treatments, minimizing financial burdens and reducing processing delays.
- Emergency Hospitalization
Cashless claims can be initiated within 24 hours of admission, while reimbursement is available if pre-authorization approval is delayed.
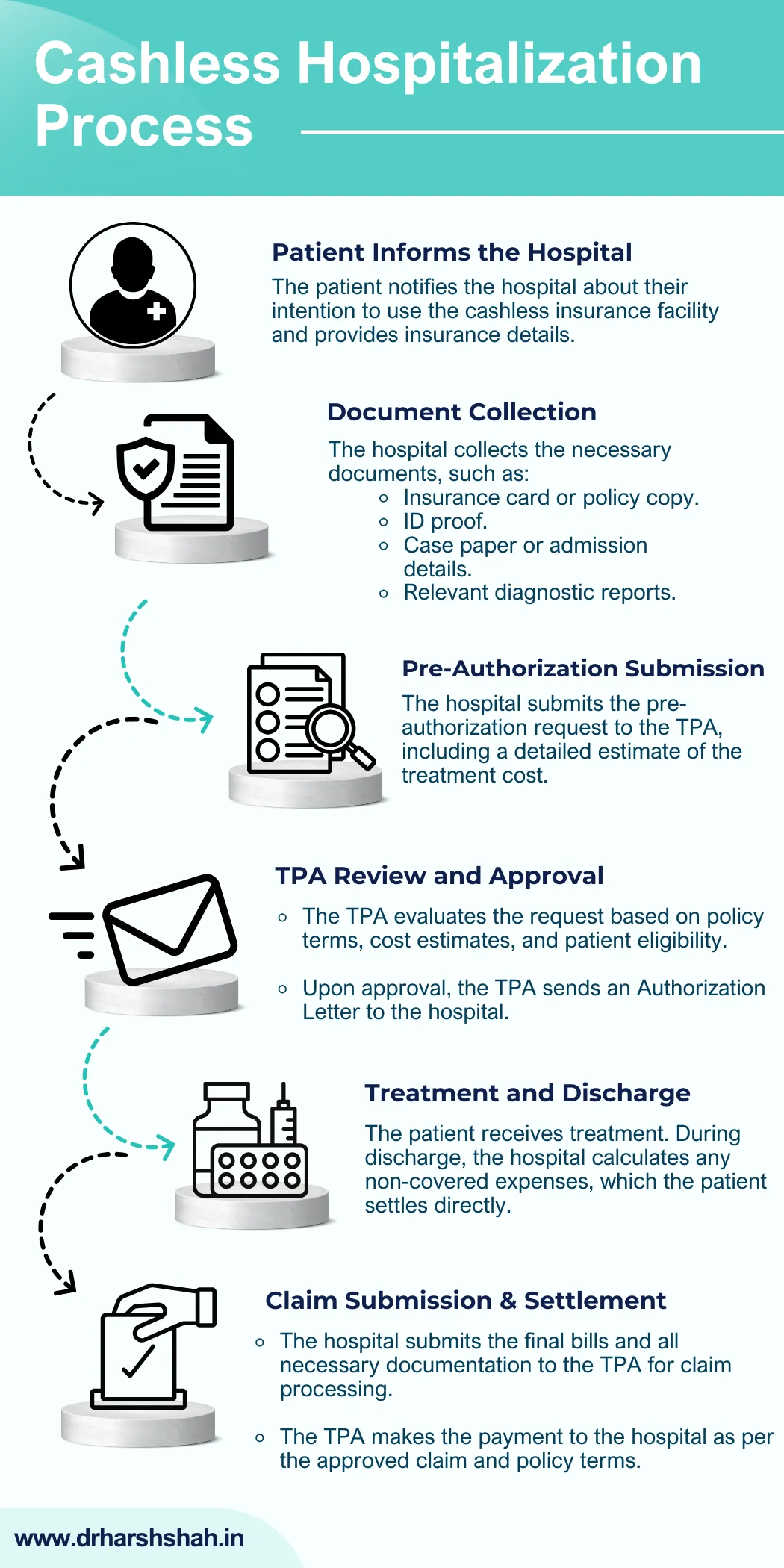
How Cashless Hospitalization Works at Apollo Hospitals?
How to Prepare for Planned Hospitalization with Insurance?
- Verify Your Insurance Policy Coverage
⦿ Understand Coverage: Carefully review your insurance policy to confirm that your planned treatment is included. Check for exclusions, co-payments, and coverage limits specific to your procedure.
⦿ Check Network Hospitals: Ensure that the chosen hospital, such as Apollo Hospitals, is part of your insurer’s network, allowing you to benefit from cashless facilities.
⦿ Confirm Eligibility: Verify that your policy is active and meets the waiting period or other prerequisites necessary for the planned treatment.
- Prepare Essential Documents
Having all required documents organized is vital for a smooth insurance process. Here’s a checklist:
⦿ Insurance Card: A valid insurance card issued by your provider for claim validation.
⦿ ID Proof: A government-issued identification document (e.g., Aadhaar card, passport, or driver’s license).
⦿ Policy Details: A copy of your insurance policy or policy number for easy reference.
⦿ Medical Documents:
– Doctor’s prescription recommending hospitalization.
– Diagnostic reports and supporting case papers.
– Detailed medical history, if applicable, to substantiate the claim.
- Obtain Pre-Authorization for Treatment
Pre-authorization is mandatory for cashless hospitalization and must be obtained well in advance for planned treatments.
⦿ Submit a Pre-Authorization Form: Fill out the insurer’s or TPA’s pre-authorization form, which includes details of the treatment and estimated costs. The hospital’s insurance cell can assist in completing and submitting this form.
⦿ Provide Supporting Documents: Include all required medical reports and doctor’s recommendations with the form.
⦿ Follow Up: Regularly check the status of your pre-authorization request to ensure timely approval.
- Plan for Non-Covered Expenses
While most major expenses are included in cashless hospitalization, some costs may need to be covered by the patient.
⦿ Non-Medical Items: Prepare for charges like consumables, registration fees, or room upgrades, which are not covered by insurance.
⦿ Co-Payment or Deductibles: Review your policy for any co-payment requirements or deductibles that you may need to pay.
- Stay Informed About Claim Limits and Approval Timelines
Understanding your policy’s coverage and processing timelines helps avoid surprises.
⦿ Understand Claim Limits: Ensure the estimated treatment cost fits within your policy’s insured sum, including any sub-limits.
⦿ Approval Timelines: Pre-authorization usually takes 24-48 hours. Submit your documents early to prevent delays in treatment.
- Confirm Hospital Coordination
Smooth coordination between the hospital and insurer is crucial for hassle-free claims.
⦿ Insurance Desk Support: Apollo Hospitals’ insurance cell ensures all required documents are submitted and coordinated efficiently.
⦿ Emergency Contacts: Keep your insurer’s helpline and the hospital’s insurance desk contact handy for quick assistance in case of any issues.
Role of Third Party Administrators (TPAs) in Cashless Insurance
Streamlining Insurance Claims
⦿ TPAs oversee the entire insurance claim process, from verifying patient eligibility to processing approvals efficiently.
⦿ They act on behalf of insurance companies to validate treatment coverage in accordance with policy terms.
Pre-Authorization for Cashless Treatment
⦿ TPAs review pre-authorization requests submitted by the hospital for planned or emergency treatments.
⦿ They assess the documents, medical reports, and estimated costs to confirm if the treatment falls under the insurance policy's coverage.
Streamlining Insurance Claims
⦿ TPAs oversee the entire insurance claim process, from verifying patient eligibility to processing approvals efficiently.
⦿ They act on behalf of insurance companies to validate treatment coverage in accordance with policy terms.
Pre-Authorization for Cashless Treatment
⦿ TPAs review pre-authorization requests submitted by hospitals for both planned and emergency treatments.
⦿ They assess medical reports, supporting documents, and estimated costs to confirm if the treatment qualifies under the insurance policy’s coverage.
Coordination with Hospitals
⦿ TPAs maintain a network of hospitals, including Apollo Hospitals, to facilitate cashless hospitalization at designated facilities.
⦿ They enable seamless communication between hospitals and insurers, ensuring timely approvals and reducing delays.
Verifying Policy Coverage and Eligibility
⦿ TPAs verify policy details, such as coverage limits, waiting periods, and exclusions for pre-existing conditions, ensuring claims meet policy guidelines.
⦿ They maintain transparency by keeping all stakeholders informed about claim status and coverage specifics.
Coordination with Hospitals
⦿ TPAs maintain a network of hospitals, including Apollo Hospitals, to facilitate cashless hospitalization at designated facilities.
⦿ They enable seamless communication between hospitals and insurers, ensuring timely approvals and reducing delays.
Verifying Policy Coverage and Eligibility
⦿ TPAs verify policy details, such as coverage limits, waiting periods, and exclusions for pre-existing conditions, ensuring claims meet policy guidelines.
⦿ They maintain transparency by keeping all stakeholders informed about claim status and coverage specifics.
Processing Final Claims
⦿ After treatment, TPAs review the hospital’s final bill and supporting documents to process claims for settlement with the insurer.
⦿ They ensure approved claims are settled directly with the hospital, while patients are informed about any non-covered expenses.
Resolving Patient Queries
⦿ TPAs provide dedicated helplines to assist patients with claim-related queries, document submissions, and policy clarifications.
⦿ They guide patients through the claim process, ensuring a clear understanding of procedures and requirements.
Processing Final Claims
⦿ After treatment, TPAs review the hospital’s final bill and supporting documents to process claims for settlement with the insurer.
⦿ They ensure approved claims are settled directly with the hospital, while patients are informed about any non-covered expenses.
Resolving Patient Queries
⦿ TPAs provide dedicated helplines to assist patients with claim-related queries, document submissions, and policy clarifications.
⦿ They guide patients through the claim process, ensuring a clear understanding of procedures and requirements.

Need More Information About Cashless Hospitalization for Cancer Treatment?
Frequently Asked Questions
In case of delays, you may need to pay upfront and later apply for reimbursement. Apollo assists with quick documentation to expedite the process.
Yes, cashless insurance can be utilized for emergency cancer treatment. Submit the required documents within 24 hours of admission to initiate the process.

