Esophagectomy
A Complete Guide to Food Pipe Removal Surgery in India
You are here >> Home > Blog > Cancer > Cancer Surgery > Surgery English > Esophagectomy
Facing a major surgery can feel overwhelming. If you or a loved one has been advised to undergo an Esophagectomy, you probably have a million questions. What is it? Why is it needed? What happens during and after the surgery? This guide is here to answer all your questions in simple, easy-to-understand language. We will walk you through everything you need to know about this life-changing procedure, from the different types of surgery to life after recovery.
Summary
- What is an Esophagectomy?
In this surgery, the diseased part of the esophagus is removed.
⦿ The goal is to remove the cancer or damaged part and allow eating again.
- How the Surgery is Done
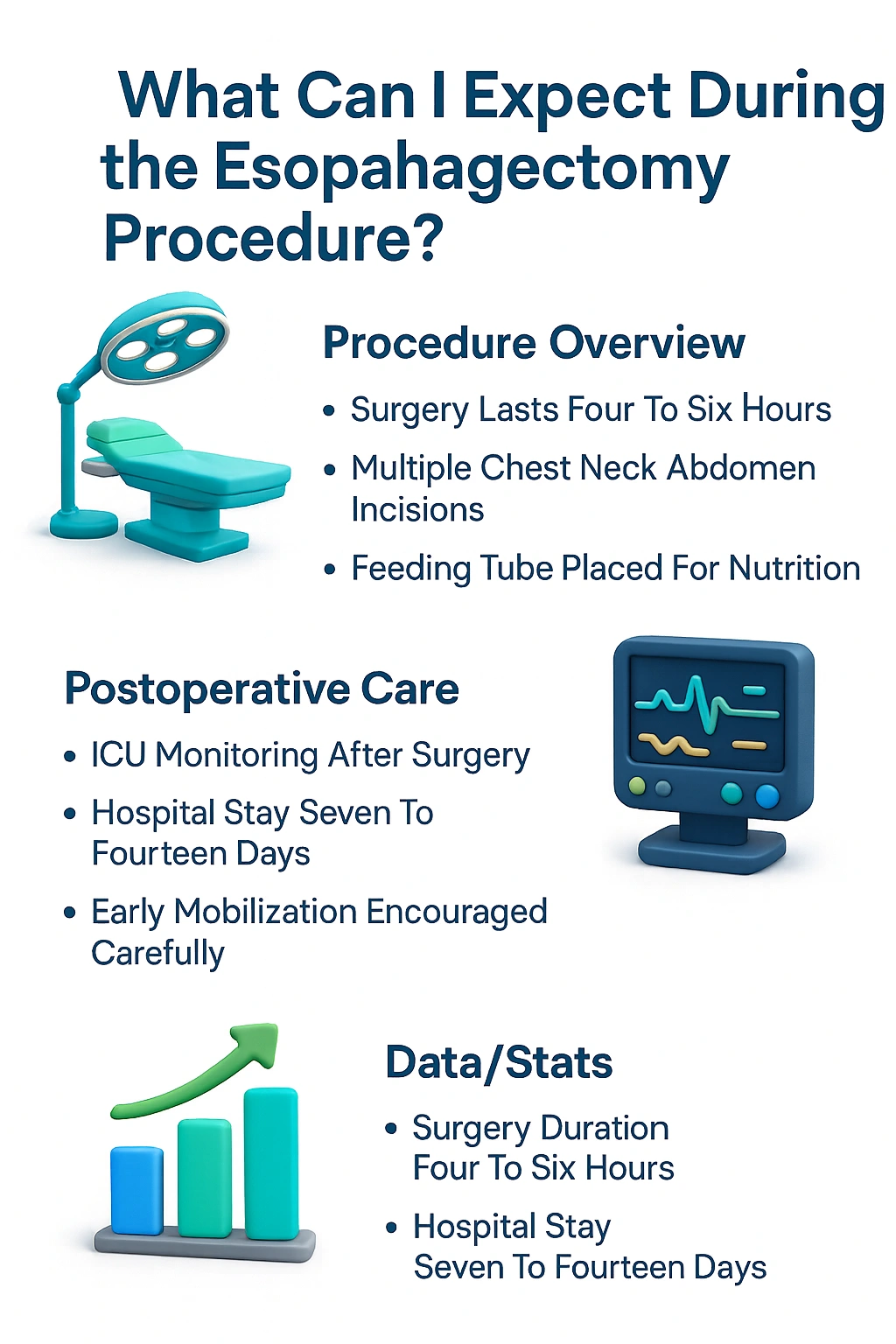
⦿ It is done under general anesthesia and can take many hours.
⦿ Patients usually stay in ICU first for close monitoring.
- Recovery and Lifestyle
⦿ Weight loss, acid reflux, and small frequent meals are common after surgery.
⦿ Regular follow-up, chest exercises, and a healthy lifestyle help long-term recovery.
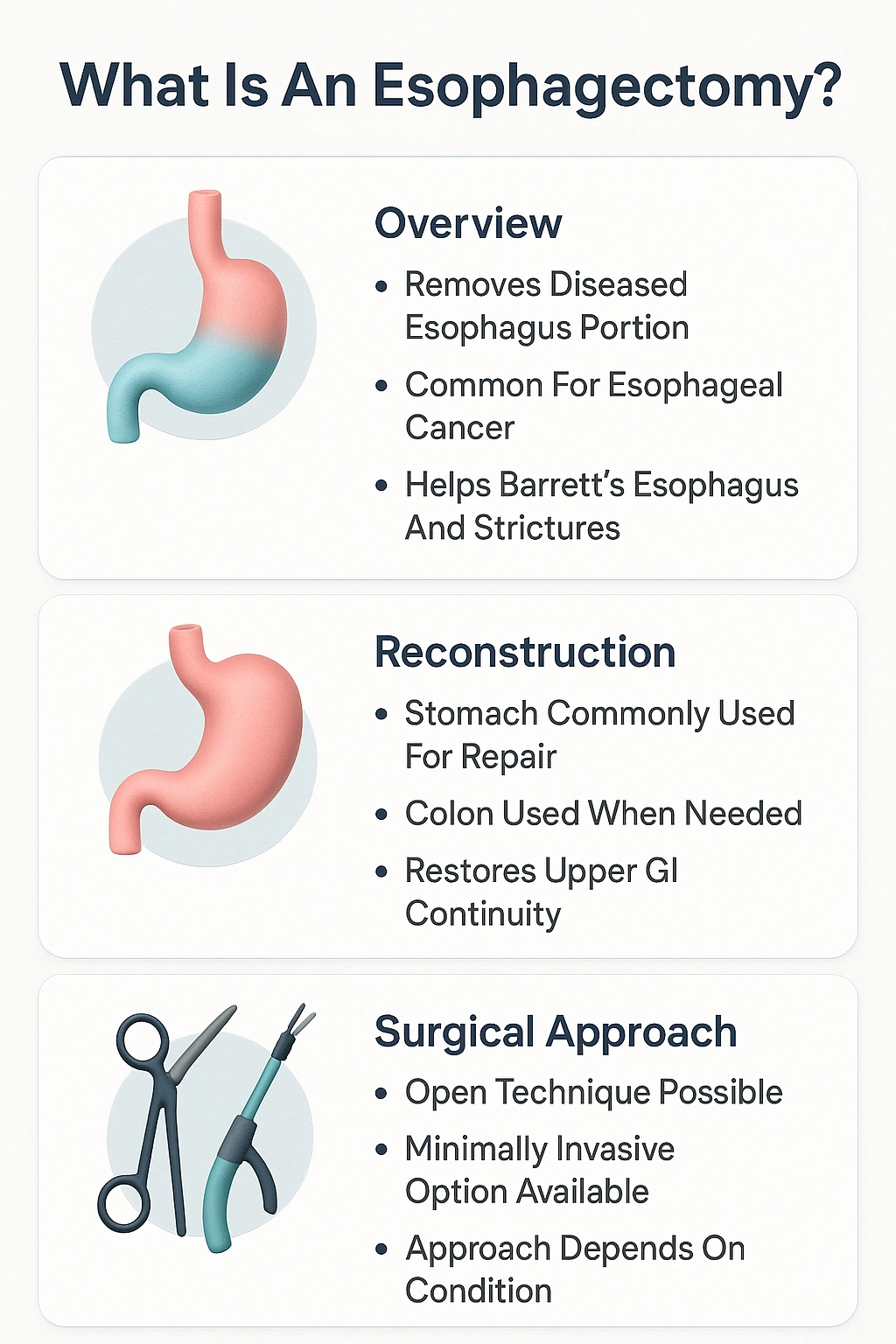
What is Esophagectomy ?
History of Esophagectomy
Types of Esophagectomy Surgery
- Transhiatal Esophagectomy (THE)
Imagine a tunnel being made without breaking the mountain. That’s similar to a Transhiatal Esophagectomy. This surgery is performed through incisions in the neck and the abdomen. The surgeon works through these two points to free the esophagus and remove it, avoiding a large cut in the chest. This generally means less pain and a quicker recovery from a breathing perspective. The detailed transhiatal esophagectomy steps involve careful dissection behind the breastbone to pull the esophagus out.
- Transthoracic Esophagectomy (TTE)
- Minimally Invasive Esophagectomy (MIE)
- Open Esophagectomy
- Comparing Different Esophagectomy Approaches
| Feature | Transhiatal Esophagectomy (THE) | Transthoracic Esophagectomy (TTE) | Minimally Invasive Esophagectomy (MIE) |
|---|---|---|---|
| Incisions | Neck and Abdomen | Chest and Abdomen (and sometimes neck) | Several small "keyhole" incisions |
| Best For | Tumors in the lower esophagus | Tumors in the upper and middle esophagus | Medically fit patients with early-stage tumors |
| Main Advantage | Avoids a large chest incision, less lung-related issues | Excellent view for complete tumor and lymph node removal | Less pain, faster recovery, smaller scars |
| Main Disadvantage | Limited view of the upper esophagus and lymph nodes | More stressful on the lungs, potentially longer recovery | Technically demanding, requires specialized skills and equipment |
Indications for Esophagectomy
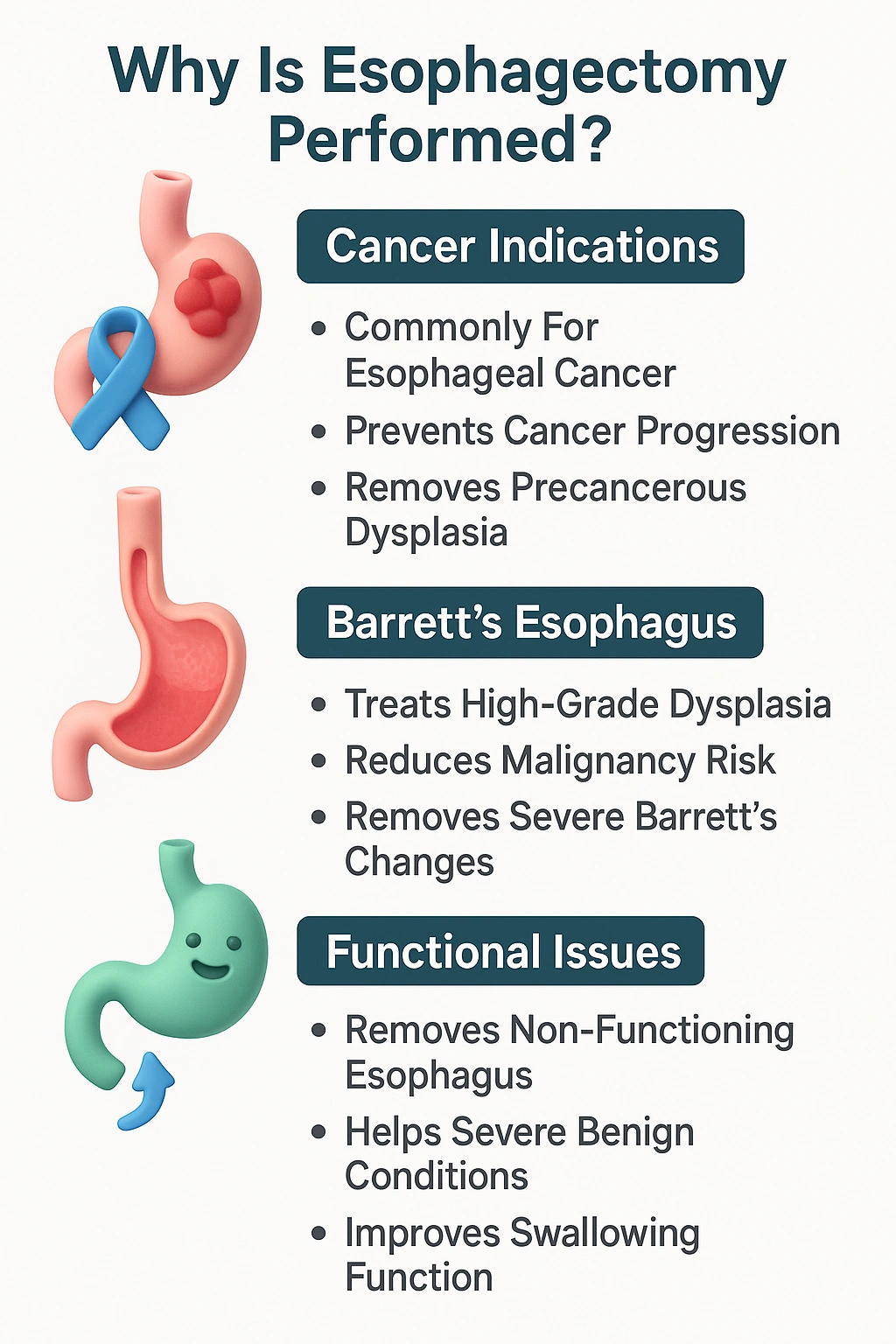
- Esophageal Cancer
- Barrett’s Esophagus with High-Grade Dysplasia
Barrett’s esophagus is a condition where the lining of the esophagus changes, usually due to long-term acid reflux. Over time, these changed cells can become pre-cancerous (a condition called dysplasia). When high-grade (severe) dysplasia is found, it means the cells are very close to turning into cancer. An Esophagectomy may be recommended to remove this tissue and prevent cancer from developing.
- Esophageal Strictures or Injury
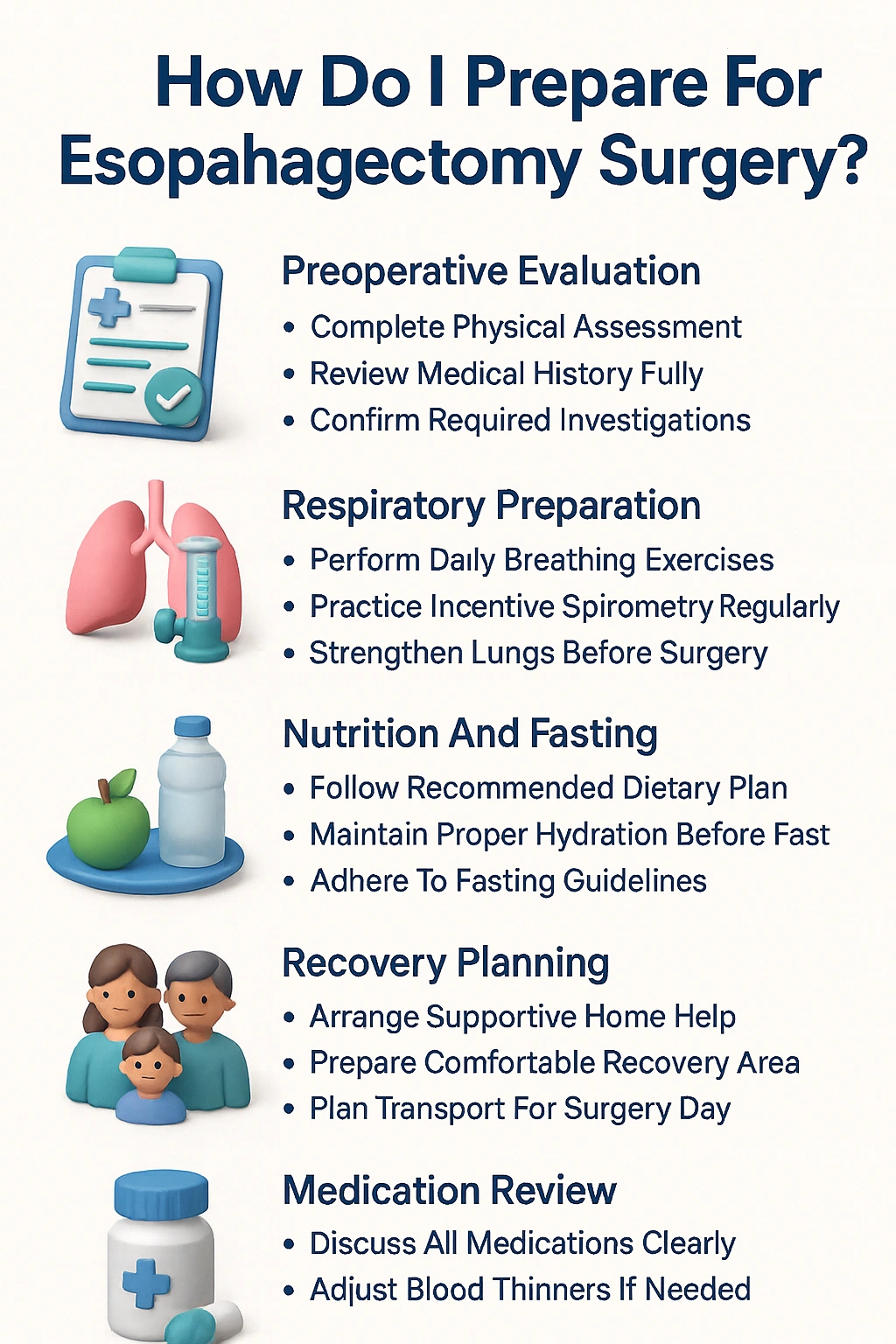
Preoperative Evaluation and Preparation
- Diagnostic Imaging
⦿ CT Scan: This creates a detailed 3D picture of your chest and abdomen, showing the size of the tumor and whether it has spread to nearby lymph nodes or organs.
⦿ PET-CT Scan: This scan is even more sensitive. A special sugar dye is injected, which cancer cells absorb more than normal cells. This helps to find even small spots of cancer anywhere in the body.
⦿ Endoscopic Ultrasound (EUS): A thin tube with an ultrasound probe is passed down your throat. This gives a very close-up view of the tumor and shows how deep it has grown into the wall of the esophagus and if it has spread to nearby lymph nodes.
- Nutritional Assessment
- Pulmonary Function Tests
- Cardiac Evaluation
Esophagectomy Procedure – Step by Step
- Anesthesia and Positioning
- Esophageal Removal
- Reconstruction
After the esophagus is removed, the food pathway needs to be rebuilt. This is a critical part of the Esophagectomy. The esophagectomy anatomy is permanently changed here.
⦿ Esophagectomy gastric pull through: This is the most common method. The stomach is reshaped into a tube, pulled up into the chest (or neck), and connected to the remaining part of the esophagus.
⦿ Esophagectomy colonic interposition: If the stomach cannot be used (for example, due to previous surgery or disease), a piece of the colon (large intestine) is used to create a new food pipe.
- Lymph Node Dissection
Cancer cells can travel through lymph channels. The surgeon will remove the lymph nodes near the esophagus. This is a crucial step because examining these nodes under a microscope helps determine the exact stage of the cancer and tells the doctors if further treatment, like chemotherapy, is needed after the Esophagectomy.
Postoperative Care and Recovery
- ICU Monitoring
After surgery, you will be taken to the Intensive Care Unit (ICU). Here, nurses and doctors will closely monitor your heart rate, blood pressure, oxygen levels, and breathing. You will receive pain medication to stay comfortable. You might have a breathing tube for a short while.
- Early Mobilization
It might seem difficult, but getting out of bed and walking as soon as possible is very important. Even sitting in a chair helps. This prevents serious complications like blood clots in the legs (DVT) and lung infections (pneumonia).
- Gradual Diet Progression
- Nutritional Support
- A Typical Post-Esophagectomy Diet Progression Plan
| Stage | Time After Surgery (Approx.) | What You Can Have | Important Notes |
|---|---|---|---|
| Stage 1: NPO | Days 1-5 | Nothing by mouth (Nil Per Oral) | All nutrition is given through an IV line or feeding tube. |
| Stage 2: Clear Liquids | Days 5-7 (after a swallow study) | Water, clear soups, clear juices, tea without milk | Start with small sips. Your medical team will monitor for any issues. |
| Stage 3: Full Liquids / Pureed | Week 2 | Thin soups, yogurt, milkshakes, khichdi, dal (blended smooth) | Focus on high-protein options. Eat slowly and in small amounts. |
| Stage 4: Soft Diet | Weeks 3-6 | Soft cooked vegetables, minced meat, soft fruits, idli, paneer | Chew everything very well. Avoid hard, dry, or sticky foods. |
| Stage 5: Modified Regular Diet | After 6 weeks | Gradually return to a more normal diet | Continue eating 5-6 small meals a day. Sit upright during and after meals. |
Risks and Complications
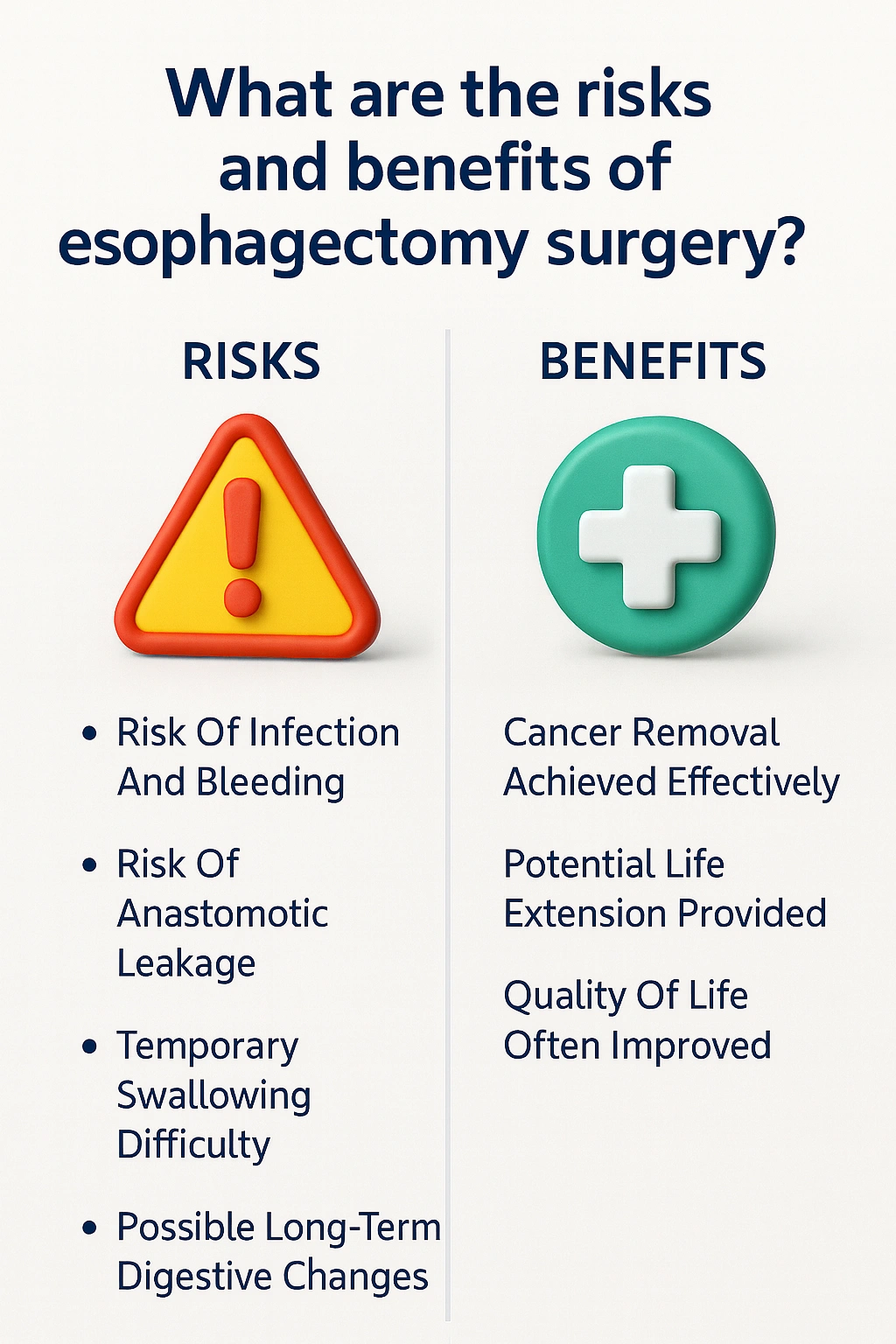
- Anastomotic Leak
- Pulmonary Complications
The lungs are very close to the esophagus, and the surgery can affect them. Pneumonia (lung infection), fluid buildup around the lungs (pleural effusion), and breathing difficulties are some of the most common complications after an Esophagectomy.
- Vocal Cord Injury
- Stricture Formation
- Warning Signs of Complications Post-Esophagectomy
| Symptom | Possible Complication | What to Do |
|---|---|---|
| Fever, chest pain, rapid heart rate, feeling very unwell | Anastomotic Leak | Contact your doctor or go to the emergency room immediately. This is a medical emergency. |
| Coughing, shortness of breath, fever, yellow/green phlegm | Pneumonia (Lung Infection) | Inform your medical team right away. You may need antibiotics and breathing exercises. |
| Difficulty swallowing that gets worse over time | Stricture Formation | Inform your doctor. You may need an endoscopy and dilation. |
| Sudden, severe pain, swelling, or redness in one leg | Deep Vein Thrombosis (DVT) | Seek immediate medical attention. This is a serious condition that can lead to a pulmonary embolism. |
| Hoarseness or a weak, breathy voice | Vocal Cord Injury | Mention it to your surgeon during follow-up. A speech therapist may be able to help. |
Life After Esophagectomy
- Eating and Swallowing Changes
Your new “stomach” in your chest is much smaller than your original one. This means you will feel full very quickly. You will need to eat 5-6 small meals a day instead of 3 large ones. It is very important to:
⦿ Eat slowly and chew your food thoroughly.
⦿ Sit upright while eating and for at least an hour afterward to prevent reflux.
⦿ Avoid drinking large amounts of fluid with your meals.
- Weight Loss and Nutritional Challenges
- Long-Term Monitoring
Survival Rates and Prognosis
- Based on Stage of Cancer
- Impact of Complete Resection
- Importance of Adjuvant Therapy
Frequently asked questions

Dr. Harsh Shah
MS, MCh (GI cancer Surgeon)
Dr Harsh Shah is a well known GI & HPB Robotic Cancer Surgeon in Ahmedabad. He treats cancers of Esophagus, stomach, liver, pancreas, colon, rectum & small intestines. He is available at Apollo Hospital.

